Hyperparathyroidism in A-bomb Survivors: An Update
Results relating hyperparathyroidism to A-bomb exposure have stimulated close monitoring for this condition during RERF’s Adult Health Study examinations. New data are presented.
by Saeko Fujiwara, Department of Clinical Studies, RERF
This article was originally published in RERF Update 2(4):5, 1990.
Since the mid-1970s, hyperparathyroidism (HPT) induction has been associated with radiotherapy of the head and neck region. Interestingly, during the past few years, results from RERF’s Adult Health Study (AHS) biennial examinations have begun to reveal a possible relationship between HPT and A-bomb radiation exposure, thus suggesting that relatively low-dose exposure may also induce this disorder.
A study conducted at RERF from August 1986 through July 1988 on 4,675 persons aged 41 or older showed that HPT was more prevalent among A-bomb survivors who received higher radiation doses (test of linear trend, p < .001), and the effect of radiation exposure was greater among individuals exposed at a younger age (p < .05) (Fujiwara et al., RERF TR 8-90). The relative risk of developing HPT at 1 Gy was 4.38 in all age groups combined, 11.1 in those 0-9 years of age at the time of the bombing (ATB), and 2.75 in those > 20 years old ATB (see Figure). Although no difference in radiation effect between the sexes was noted, females exhibited a threefold higher overall prevalence of HPT than males.
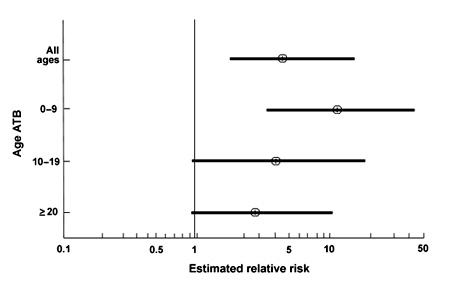
Figure. Among AHS participants, the estimated relative risk of hyperparathyroidism at 1 Gy is shown by age at the time of the bombing (ATB), 1986-1988 (point estimates and 95% confidence interval for the relative risk).
Here we will summarize new HPT data accumulated since August 1988.
Diagnosis of HPT
HPT, a generalized disorder of calcium and phosphate metabolism resulting from an increased secretion of parathyroid hormone, is caused by adenoma in approximately 82-85% of cases, by hyperplasia in 15%, and by cancer of the parathyroid gland in a small percentage of cases.
In 1986, acquisition of an autoanalyzer enabled cost-effective blood chemical measurements to be routinely undertaken as part of RERF’s biennial AHS examinations. Thereafter, HPT diagnosis has been determined biochemically, based upon the presence of consistent hypercalcemia (Ca > 10.3 mg/100 ml), accompanied by an elevated level of serum parathyroid hormone (> 520 pg/ml).
New data since August 1988
Persons newly suspected of having HPT were found more frequently in the > 1 Gy group. From August 1988 through July 1990, 12 subjects were thought to have HPT, including one female who had been in utero ATB. At a previous HPT screening conducted from 1986-88, six of these individuals had exhibited borderline levels ranging between 9.9 and 10.2 mg/100 ml of serum calcium.
The number of HPT cases by thyroid dose category is shown in the table.
|
Figure. AHS Hyperparathyroidism cases: 1986-1990
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| *No.of AHS participants tested for serum calcium |
We are somewhat concerned about the characteristically fluctuating nature of serum calcium levels that in borderline HPT cases may be below the “cutoff” point of 10.3 mg/100 ml at the time of screening. These AHS participants are not requested to return within a few days for a more conclusive parathyroid hormone screening and are therefore lost to HPT follow-up until the next cycle of biennial AHS examinations. If the prevalence rate of such borderline cases is higher among the high-dose groups than in the non-exposed group, we may be underestimating the effects of radiation exposure.
To further investigate the significant linear relationship between radiation exposure and the serum calcium level found in the AHS participants covered in the 1986-1988 survey (common slope, 0.073 ± 0.018 mg/100 ml/Gy), we decided to measure the PTH level of 1,600 subjects selected at random from Hiroshima AHS participants (Fujiwara et al., RERF RP 2-89). A more definitive HPT indicator, PTH screening is costly and is usually undertaken at RERF only when clear-cut hypercalcemia is diagnosed.
From May 1989 to August 1990, we found four patients who showed PTH levels indicative of HPT, i.e., >1,000 pg/ml. They had not been suspected of having HPT at either the 1986-1988 or 1988-1990 screening exams because they showed borderline calcium levels ranging from 10.0-10.1 mg/100 ml, thus indicating that some HPT cases might have an upper but normal range of serum calcium. As noted with the recent hypercalcemia cases, the thyroid dose for three of these individuals was greater than 1 Gy.
Thus, using two biochemical techniques, HPT is being diagnosed even in asymptomatic A-bomb survivors. Follow-up for HPT diagnosis in borderline hypercalcemia patients will help determine the clinical features of such cases and whether they were actually induced by radiation exposure.

